Testicular Cancer
Testicular cancer is the disease condition where malignant cancer cells are noted in the testicles, the male’s gonads or sex glands and are often felt as painless lumps. These gonads are placed inside a sac (scrotum) and are responsible for the production and storage of sperm cells. Additionally, they are the chief source of the male hormones, testosterone, that influence the maturity of the reproductive organs and the development of other physical characteristics in males.
Matched up to other cancer types, testicular cancer is quite rare but is considered to be the most common type afflicting American males between 15 and 34 years old. The cancer is classified into two forms, basing on the type of cells present: seminomas which account for 30% of the condition and non-seminomas, the most common type (70%). Early diagnosis helps make this cancer treatable but even if it has metastasized, treatment options are still easy compared to other types. Metastasis often occurs through the lymph nodes and blood.
Seminomas, made of undeveloped germ cells, are subdivided into: anaplastic, spermatocytic or classic. These cells develop slowly and are more localized in the testicles.
Non-seminomas would include embryonal carcinoma, choriocarcinoma, yolk sac tumors or teratoma. Testicular tumor cells may contain both types. These cells evolved from specialized mature germ cells and are more likely to be more damaging than the seminomas.
Symptoms of Testicular Cancer
Testicular cancer symptoms and signs are not necessarily particular to the disease. A number of other conditions can cause them. The first testicular cancer symptom is usually a painless swelling of either of the testicles or the presence of a painless lump the size of a pea. Men are urged to check their testicles regularly to detect the cancer early. Some of the men who have this problem are asymptomatic in the early stages. Testicular cancer symptoms and signs are usually detected accidentally during scheduled physical exams.
There are a number of testicular cancer cells (germ cell tumors) that can produce elevated concentrations of human chorionic gonadotropin (HCG) hormone that will stimulate breast development in men. Blood tests can determine the levels of HcG in the blood and this is important especially in the diagnosis and staging of the cancer.
Even if the cancer cells have metastasized, about 25% of the male population who has this disease would experience any of the testicular cancer symptoms and signs before being diagnosed positive. The most frequent area for metastasis is the lymph nodes at the posterior portion of the abdomen thus a late testicular cancer symptom is lower back pain. If the cancers cells have reached the lungs, pulmonary symptoms such as cough, shortness of breath, hemoptysis or chest pain are noticed.
Signs of Testicular Cancer
A summary of the testicular cancer signs that men should look out for are:
- A painless lump in one or both testicles which may be pea-sized or as large as an egg or marble
- Enlargement or a considerable shrinking of the testicle
- An alteration on the testicle’s consistency (hardness)
- Scrotum feels heavy
- Dull ache at the groin or hypogastric area
- An abrupt accumulation of fluid inside the scrotum
- Tenderness in the testicles or scrotum
- Enlargement or soreness of the breast
If most of these testicular cancer signs are felt for over two weeks, it is recommended that further diagnostic exams be made to ensure early detection of the disease.
How to check for testicular cancer
Testicular self-examination should be done monthly beginning at 15 years old. Checking for testicular cancer should be done regularly to allow men to become familiar with their body hence could detect changes early.
Checking for testicular cancer should be done after a warm shower or bath as heat would cause the scrotum to relax, making it much easier to detect any abnormalities.
To start checking for testicular cancer, try to stand before a mirror and check if there is any swelling on the skin of the scrotum. With both hands, inspect each testicle. Place the thumb on top while the middle and index fingers are placed underneath the testicle. Gently roll the testicle between these fingers. No pain should be felt when this is being done. Keep in mind that one of the testicles is normally larger than the other.
Next, try to locate the epididymis, the tube-like structure at the back of the testicle. This soft structure collects and moves the sperms. Some of the men would mistake this for a lump but cancerous lumps are usually located at the sides or front part of the testicles.
If you do find a lump or any testicular cancer signs, then have them checked by a doctor even if you are still doubtful. It is better to have it checked by a professional than hoping that it is not cancerous.
What does testicular cancer look like?
Histologically, the malignant testicular cancer cells have profuse whitish protoplasm rich in glycogen. The nuclei are irregular and large with prominent nucleoli or two. The largest part of testicular germ cell tumors has numerous chromosomes that are triploid or tetraploid. About 80% of these have an isochromosome 12p (the short arm).
Testicular Cancer Pictures
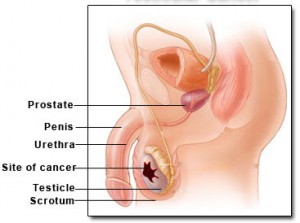
Picture 1 : Site of testicular cancer
Picture 2 : Seminoma of the testis
Causes of Testicular Cancer
What causes testicular cancer is still unknown. But there are people who are more prone to develop this type of cancer.
- Individuals with a positive history of testicular cancer in their family
- Diagnosed cancer in one of the testicle
- Smoking
- Cryptorchidism (undescended testes)
- Caucasian ( five times more in white men than in any other groups)
- Mumps affecting testes
- Congenital abnormalities such as inguinal hernia
- HIV
- Klinefelter’s syndrome —genetically underdeveloped testicles
Some researchers have suggested that infertility is one of the probable testicular cancer causes but this has not yet been established. There is no correlation between vasectomy, trauma or diet and testicular cancer.
A new research has suggested that taller men have a higher risk of developing testicular cancer. For every extra five centimeters (2 inches) in height, the risk increases by thirteen percent.
Testicular Cancer Statistics
According to the American Cancer Society, in 2010, approximately 8,480 American males were diagnosed with testicular cancer. It was estimated that around 350 of these men will die because of the disease, mostly from metastasis that were not successfully treated with radiation therapy, chemotherapy or surgery.
Most testicular cancer cases are from men between 15 and 54 years old. This is not common; in a man’s lifetime the probability of acquiring it would be around 1 in every 270 and the threat of dying because of it is about 1 in every 5,000.
In the US, it is estimated that 7,500 men each year, 625 men each month and 144 men each week will have testicular cancer. In the UK, around 2000 males are diagnosed to have this disease each year and every year, 70 men die due to this disease.
Testicular Cancer Prognosis
There has been a lot of progress in the battle against testicular cancer. In the 70s, around 90 percent of diagnosed patients with metastasis died because of the disease. However, in 1990, these numbers have gone down especially when chemotherapy drugs like Cisplatin were introduced. Now, almost 90% of the men with metastasized testicular cancer are cured and the survival rate has increased.
The outlook for this disease is good and the earlier it is diagnosed, the better are the chances of survival. Although there might recurrences of the disease, careful monitoring would help improve the chances of catching the disease before it can go out of hand. Statistics have shown that it is during the first year after treatment that the disease has a high probability of recurring.
Testicular Cancer Screening
A standard screening test for testicular cancer is not available. Most of the time, the presence of this disease are discovered by the men themselves through self-examinations or by accident. Occasionally, the problem is detected by a doctor during a routine physical exam.
Testicular Cancer Staging
Staging is a system of describing where the cancer has metastasized. Different diagnostic exams are used to accurately determine the stage of the testicular cancer. Identifying the stage would help the doctor plan the treatment care the patient will undergo and helps foresee the prognosis of the patient.
Two types of staging are done for testicular cancer: pathological staging and clinical staging. Clinical staging is based on the results of the diagnostic exams such as x-rays or CT scans. Pathological staging, on the other hand, is based on the microscopic evaluation of the cells removed through surgery.
The TNM system is often used to describe the stages. This system uses three different criteria: the location of the primary tumor, if the cancer has spread the surrounding lymph nodes and the area of metastasis.
Stage 1: the cancer is confined or localized at the testicles
- Stage IA : cancer is in the testicles and epididymis, and may have extended to the inner layer of the testicular membrane but all the tumor markers are within normal limits
- Stage IB: testicles, epididymis and the testicular lymph nodes or blood vessels; or to the outer layer of testicular membrane; or in the scrotum or spermatic cord. All tumor markers within normal limits
- Stage IC: found anywhere the spermatic cord, testicles or scrotum. All tumor markers slightly elevated or one marker is rather above normal.
Stage 2: the cancer has metastasized to the retroperitoneal lymph nodes (posterior portion of the abdomen just below the diaphragm and in between the two kidneys.
- Stage IIA: is anywhere inside the spermatic cord, scrotum or testicle, and has expanded up to five lymph nodes within the abdomen, none bigger than two centimeters. Every tumor marker levels are either normal or a little above normal.
- Stage IIB: cancer is somewhere inside the scrotum, testicle or spermatic cord; and either: has metastasized up to five lymph nodes within the abdomen; no less than one lymph node is bigger than two centimeters, however, none are bigger than five centimeters; or has metastasized to over five lymph nodes and the nodes are no bigger than five centimeters. Every tumor marker levels are either normal or a little above normal.
- Stage IIC: cancer is somewhere inside the scrotum, testicle or spermatic cord; and has metastasized to one lymph nodewithin the abdomen that is bigger than five centimeters. Every tumor marker levels are either normal or a little above normal
Stage 3: the cancer has metastasized to the remote sites including the brain, liver, bones and lungs. The tumor marker levels may range from normal to elevated.
Testicular Cancer Survival Rate
The rate at which these men with testicular cancer will survive five years from diagnosis and treatment is 95%. For men who have no signs of metastasis, the survival rate is increased to 99%. For those who are at stage 2 (metastasis to the posterior portion of the abdomen), survival rate is 96%.
Patients who are at good-risk stage 3 (more extensively spread), the survival rate is 90 to 94% while those at the intermediate-risk stage 3 have 79 to 83% survival rate and those at the poor-risk stage 3 group have an overall survival rate of 48 to 71%. Though the survival rate is quite low, these men are still curable.
These survival statistics should be cautiously interpreted since these results are based on the thousand diagnosed cases in the US every year. The actual individual chances may vary.
Testicular Cancer Prevention
There is no definite approach in testicular cancer prevention since most of the risk factors are beyond a person’s influence. Several doctors would recommend regular self-examination of the testicles to identify the problem earlier on. Although, there are some who would not agree to this. Therefore, it is better to discuss this with the doctor.
References:
http://www.nlm.nih.gov/medlineplus/testicularcancer.html
http://www.medicinenet.com/testicular_cancer/article.htm
http://www.mayoclinic.com/health/testicular-cancer/DS00046
http://www.bbc.co.uk/health/physical_health/conditions/in_depth/cancer/testicularcancer1.shtml