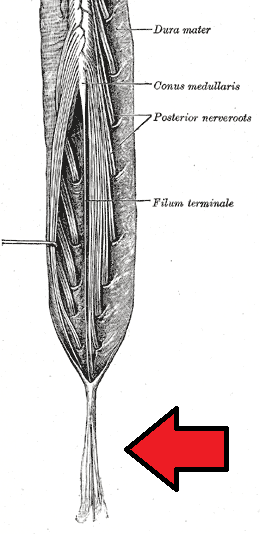
Cauda Equina syndrome or CES is a rare disease that generally is considered a surgical emergency. People diagnosed with CES experience compression on the nerve roots in their spines. One may require prompt treatment to prevent permanent damage causing incontinence and likely lasting paralysis in the legs.
CES impacts a nerve root bundle known as cauda equine, which means horse’s tail in Latin. These nerves are situated at the lumbosacral region, i.e., the bottom end of the spinal cord. They receive and transmit signals to and from one’s feet, legs, and pelvic organs.
Symptoms of this syndrome can manifest all on a sudden or may require weeks or even months to develop. The onset of CES is often illustrated using the characteristic distinctions mentioned below:
- Acute onset: Symptoms rapidly develop within twenty-four hours.
- Gradual onset: Symptoms develop progressively, and they may come and disappear over several weeks or even months.
Causes of Cauda Equina Syndrome
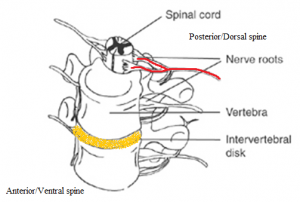
- Primary: CES typically stems from a huge herniated disc that is formed in the lumbar area of the affected Individual. A single excessive injury or strain may lead to a herniated disc. Nonetheless, it is pretty standard for the disc material to degenerate naturally as one age and the supportive ligaments start to weaken. Now, as this process of degeneration progresses, a considerably minor twisting movement or strain can cause a ruptured disk.
Other Likely Causes
- Spinal infections or inflammation (SII)
- Spinal lesions and tumors (SLT)
- Violent injuries on the lower back; such as; auto accidents, falls, gunshots
- Lumbar spinal stenosis (LSS)
- Birth abnormalities
- Spinal anesthesia
- Spinal hemorrhages; for instance; subdural, subarachnoid, epidural
- Spinal arteriovenous malformations (S-AVMs)
- Postoperative lumbar spine surgery complications (PO-LSSC)
Symptoms of Cauda Equina Syndrome
Low back pain
- Local pain: An intense, aching pain caused by an irritation in the vertebral body and soft tissue.
- Leg/radicular pain: A deep, stabbing pain triggered by compressed nerve roots; spreading in the specific areas that are controlled by such compromised nerves, and it is called a dermatomal distribution.
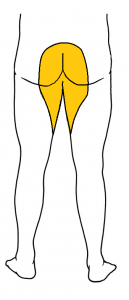
- Sciatica: AN unilateral (in one leg) or bilateral (both the legs) pain originating in the buttocks area and continues to the back of one’s legs and thighs.
- Perineal/saddle paresthesia: Loss of sensation in one’s groin or region of contact when someone is sitting or resting vertically on a saddle.
- Bowel disturbances
- Constipation
- Incontinence: Inability to experience or stop a bowel movement
- The absence of anal tone as well as sensation
- Bladder disturbances
- Urinary hesitancy: Difficulty initiating urination
- Urinary retention: Inability to urinate
- Incontinence: Inability to cease or manage urination
- Decreased urethral sensation: Decreased sensation during urination
- Absent or reduced lower extremity reflexes (LER)
- Weakness in the lower extremity muscle (LEM) and numbness
- Any sudden sexual dysfunction
Diagnosis
- Medical history: Information about the symptoms, health, and activity of the patient is obtained and scrutinized.
- Physical examination: The strength, sensation, reflexes, stability, motion, and alignment of the affected person is assessed.
- Magnetic resonance imaging (MRI)
- Computerized tomography (CT) scan
- X-ray
- Blood tests
- Myelogram: A contrast chemical is injected into the spinal cord, and its x-ray is taken to pinpoint pressure on one’s spinal cord or nerves.
Differential Diagnosis
- Amyotrophic lateral sclerosis or ALS in physical medicine and rehabilitation (ALS-PMR)
- Acute inflammatory demyelinating polyradiculoneuropathy (AIDP)
- Guillain-Barré syndrome (GBS)
- Diabetic neuropathy
- Neoplasms of the spinal cord (NSC)
- Multiple sclerosis
- Neuromuscular and myopathic complications of HIV (NMC-HIV)
- Spinal cord infections (SCI)
- Neurosarcoidosis
- Traumatic peripheral nerve lesions (TPNL)
Treatments
For a patient suffering from acute CES, surgical intervention is likely an immediate requirement. The objective is to relieve the pressure from the spinal nerves for restoring muscle function and sensation to the bladder, legs, and bowel. One of the surgical procedures mentioned below may be performed, depending upon the cause.
Discectomy
It is done to remove a part of the herniated disk, the portion which is putting pressure on the nerves. A small cut is made in the middle area on the back of the patient. The spinal muscles are relocated to expose the bony vertebra further. Then a window of the bone is cut to reveal the nerve root as well as the disc. The part impacting the spinal nerves of the affected individual is carefully removed from the ruptured disk.
Spinal Decompression
Spinal decompression is performed for cases of stenosis, where the ligaments and the bone spurs compressing the nerves are removed. A small hole is drilled in the back of the patient. The bone forming the ceiling of one’s spinal canal is removed. Then bones spurs and soft tissue are removed for creating more room to accommodate the nerves. Tumors, as well as other lesions, can be removed too.
Prevention
Prevention is concentrated on early diagnosis of the symptoms. People should be made aware of the warning signs that could potentially suggest a clinical manifestation of CES, including a change in bladder or bowel functions absence of sensation in one’s groin. However, the cases that are caused by schedule IV drug-induced infections can be prevented, and people should be cautious about not indulging in the usage of illegal schedule IV substances.
Prognosis
Using the ASIA impairment scale
Prognosis can be estimated with the help of the American Spinal Injury Association impairment scale.
- ASIA A: Ninety in every hundred patients are deemed unsuitable to undergo functional ambulation, reciprocal gait is two hundred feet or even more.
- ASIA B: Seventy-two in every hundred patients cannot achieve functional ambulation.
- ASIA C/D: Thirteen in every hundred patients fail to accomplish functional ambulation a year after the occurrence of the injury.
Using the AMI
The ambulatory motor index is also used for predicting the ambulatory capability, and an affected individual with a score of eighteen out of thirty or above has an improved likelihood for community ambulation, where the support will be restricted to a single knee-ankle-foot-orthosis (KAFO).
- A patient having a score of 23.7/30 or more may not require an orthosis.
- A patient having a score of 12/30 or less may need two KAFOs during community ambulation.
Cauda Equina Syndrome Images
References