Brugada Syndrome is a rare genetic cardiovascular disorder characterized by disturbances that affect the heart’s electrical circuitry. The primary sign is an irregularity in one’s heartbeats, and if not treated, it may potentially lead to sudden death. Present studies indicate that this syndrome could be held responsible as many as one deceased individual in every five patients who have structurally normal hearts. When a person attains adulthood, the clinical phenotype starts to manifest, and it is found to be more standard in men.
The mutant genes are transferred to the children in a process called the ADI or autosomal dominant inheritance. It indicated that only one copy of a mutated gene from the parent is required for the disease to appear in an individual. One in every two offspring of an affected person has the likelihood of one of them carrying the genetic variation, irrespective of whether one is male or female. At present, Brugada syndrome is estimated to be prevalent in one in every two thousand people.
Other Names of Brugada Syndrome
- Bangungut
- IVA
- Brugada type
- Pokkuri death syndrome (PDS)
- SUNDS
- SUDS
Causes
It is primarily caused by mutations affecting the SCN5A gene situated on chromosome three, and presently, over two hundred and fifty mutations are found to be associated with this syndrome reported in the following eighteen genes.
- SCN5A
- SCN1B
- SCN2B
- SCN3B
- SCN10A
- ABCC9
- GPD1L
- CACNA1C
- CACNB2
- CACNA2D1
- KCND3
- KCNE3
- KCNE1L -KCNE5-
- KCNJ8
- HCN4
- RANGRF
- SLMAP
- TRPM4
Symptoms
- Syncope and also cardiac arrest (happens during sleep or while resting in many patients)
- Nightmares or thrashing during night time
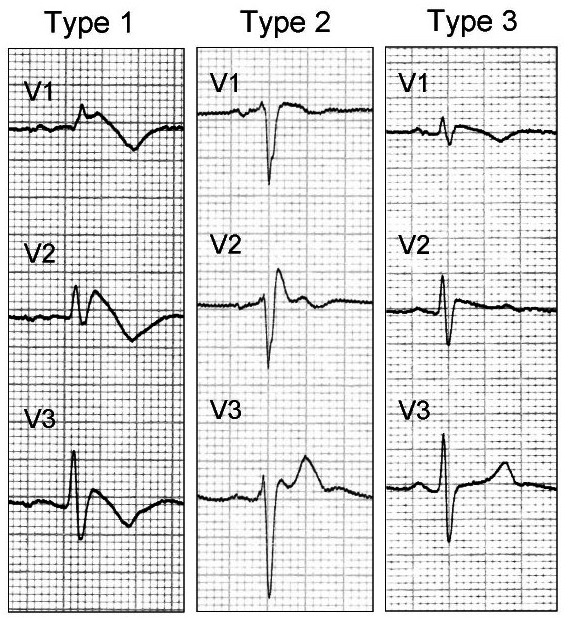
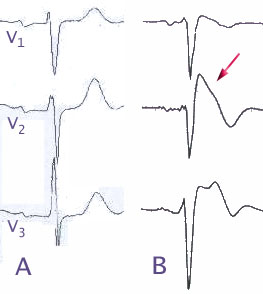
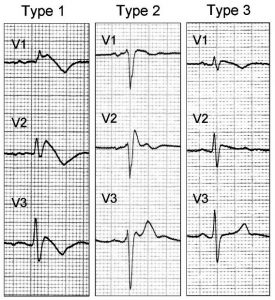
- Asymptomatic: However, a routine electrocardiogram does reveal ST-elevation in V1-V3
- Associated atrial fibrillation (AAF): Occurs in one in every five cases.
- Fever: Often reported to exacerbate or trigger clinical manifestations
The absence of a prodrome is found to be more typical for people with ventricular fibrillation documented, and this very absence is attributed to the onset of syncope in individuals with this syndrome.
Diagnosis
- Electrocardiogram (EKG or ECG): A medicine known as Flecainide or Ajmaline may be delivered intravenously during an electrocardiogram to watch how it affects the patient’s heart, and the attending doctor will look for the Brugada sign. However, not every affected individual exhibits this particular sign and such people may require multiple electrocardiograms at different times.
- Electrophysiology studies (EPS): It is typically done in CCL or cardiac catheterization laboratories.
- Blood tests for MGT or molecular genetic testing: Though DNA testing can be conducted for all genes to detect cases of mutation, only thirty to thirty-five in every hundred affected people carry an identifiable mutation in their genes. About twenty-five patients in every hundred are prescribed a sequential analysis to detect the faulty SCN5A gene in the initial stage of their genetic diagnosis.
Differential Diagnosis
- Pulmonary Embolism
- Hypothermia
- Acute Pericarditis
Treatments
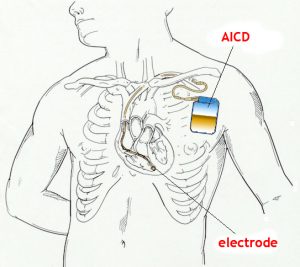
The only proven and effective therapy is an ICD or implantable cardioverter that monitors one’s heart rhythm and sends electrical impulses on demand to regulate any abnormality in a heartbeat. Some doctors prescribe Quinidine where such implantations are not viable, for instance, in neonates.
An anti-arrhythmic agent like Isoproterenol is used in cases of UVA or unstable ventricular arrhythmias (bio-electrical storms). Recommendations to treat asymptomatic patients are controversial and possible therapies to evaluate the beneficiary for an ICD placement may include performing an EPS or electrophysiologic study, examining one’s family history, or putting the concerned individual under observation until the symptoms surface, though the first symptom happens to be an SCD or sudden cardiac death in some patients in the last case.
Genetic counseling is suggested for affected persons and their family members. Other treatments are supportive and symptomatic.
Prevention
One should always remember and attempt to avoid the following triggers for reducing the odds of having a fast heartbeat.
- High temperature (380C) or fever: One should take paracetamol and seek professional advice as early as possible
- Consuming alcohol in an excessive amount: Binge drinking should be avoided
- Dehydration: A registered practitioner should be consulted in cases of persistent vomiting and diarrhea, and plenty of fluids, as well as special rehydration drinks, should be taken
- Certain Drugs: Avoiding any such medication that acts as a trigger for this syndrome
Prognosis
This syndrome can result in PVT or polymorphic ventricular tachycardia that may further degenerate, and lead to ventricular fibrillation, inducing cardiac arrest eventually. Prolonged hypoxia at the time of cardiac arrest may cause neurologic sequelae in such patients.
It is found that instances of ventricular fibrillation or sudden cardiac death occurred in eighty-two of every hundred patients diagnosed with this syndrome when a mean follow-up for two years is taken into account. A past history of syncope, a spontaneously atypical or abnormal electrocardiogram, and inducibility at the time of PES or programmed electrical stimulation (in one study) considerably increased this risk.
Aside from accidents, this syndrome may be one of the leading causes of death, in men who are less than forty years old. It is not possible to find out the true incidence because of the reporting biases. In spite of having a strong dependence for population, an estimated one in every twenty-five cases of sudden deaths, and also a minimum of one in every five incidents of sudden deaths observed in patients who have structurally normal hearts can be attributed to this syndrome. The mean age for the occurrence of sudden death is found to be twenty-six to fifty-six years for patients diagnosed with Brugada syndrome.
Brugada Syndrome Images
When to visit a doctor?
- If someone is experiencing arrhythmia (irregular heartbeat) or heart palpitations
- Facing unexplained seizures or blackouts
- Fainting
- If one’s child, parent, or sibling is diagnosed with this syndrome, the requirement for genetic testing for that individual may need to be evaluated thereafter by the general practitioner
If a close member of the family has a sudden death without any plausible cause, as this may potentially suggest the Brugada syndrome.