What is Whipple’s Disease?
Whipple’s disease is a rare gastrointestinal infectious condition, named after American pathologist, George Whipple, for his discovery of the bacteria responsible for it. He also named the disease intestinal lipodystrophy on his observation of fat and fatty acid deposits in the mucosa and lymph nodes.
Not a contagious disorder, it can prove life threatening by infecting the heart, lungs, brain, certain joints, skin and eyes.
Whipple’s Disease Signs and Symptoms
source: en.wikipedia.org/wiki/Whipple%27s_disease
The symptoms may differ from person to person and may develop slowly with the common signs including:
- Frequent watery bowel discharge or diarrhea
- Bloating and cramps felt in the abdomen that deteriorates after meals
- Weakness and dizziness that may suggest anemia
- Noticeable weight loss
- Inflammation in joints chiefly felt in the ankles, knees, wrists and elbow
- Fatigue
The less frequent symptoms are:
- Fever and chronic cough
- Breathlessness
- Leg swelling
- Darkening of the skin or hyper-pigmentation (chiefly in those areas exposed to the sun and in scars)
Central nervous system symptoms:
- Walking difficulties
- Pain in the eyes along with vision problems
- Hearing loss and a ringing sensation in the ears
- Inability to control bodily movements (ataxia)
- Jerky muscles contractions (myoclonus)
- Dementia, causing a number of problems like decreased thinking and remembering capacity
The neurological symptoms are more common in case of relapses. Rare signs may include skin rashes, while atypical cases may occur without certain symptoms like diarrhea.
Causes and Risk Factors
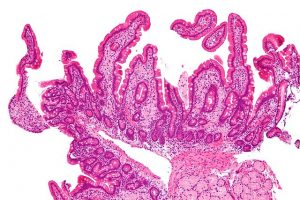
It is mainly caused by the T. whipplei bacteria which may be present in the environment, while some people may carry the bacteria, being immune to the disease themselves. The infection mostly affects the gastrointestinal system by forming internal sores or lesions and tissue thickening in the small intestine. As a result, the villi or minute finger-like projections that line the small intestine’s inside walls, become unable to absorb nutrients and participate in the breakdown of nutrients such as fats and carbohydrates, often leading to malnutrition.
Who is likely to get affected
- Older people, especially North American or European Caucasian males aged between 40-60 years
- Those with certain genetic factors that make them more susceptible to the whipplei bacteria
- Those involved in occupations like farming, and field work, as it may bring them in direct contact with the bacteria in soils or contaminated water.
Complications
- Heart and valve damage that may cause endocarditis in the long run
- Chronic recurrent meningitis
- Long lasting arthritis that may bring about cartilage damage
- Eye problems such as uveitis and occulomasticatory myorhythmia
- Limbic encephalitis that is characterized by brain inflammation
- Massive CNS infection by the bacteria may lead to permanent damage of tissues
Whipple’s Disease Tests and Diagnosis
- Physical examination: Your doctor will look for any pain or tenderness in the abdominal area, as well as search for other symptoms like skin darkening, and any edema or swelling in body tissues.
- Blood tests: A complete blood count or CBC may be ordered to determine low counts of red blood cells and the protein albumin, both indicative of anemia.
- Endoscopy: An endoscopy may be carried out by inserting a small flexible tube down the esophagus into the stomach and ultimately to the duodenum and jejunum, to closely check the intestinal lining.
- Ocular examination: May indicate inflammation of blood vessels of the eye called vasculitis.
- Biopsy: A biopsy may be ordered where a tissue sample is collected from the lining of the small bowel to be examined under a microscope. Sometime, a lymph node biopsy may also be necessary.
- Polymerase chain reaction (PCR): A diagnostic technique that helps to detect the disease by magnifying the DNA of the bacterium in saliva, gastric fluid, or intestinal fluid samples.
- Radiology: CT scan and brain MRI tests can be done to look for any central nervous system anomaly, while x-ray of the small bowel may also be performed.
PAS and electron microscopy are some other tests used for this purpose.
Differential diagnosis
- Bacterial and nonbacterial endocarditis
- Eosinophilic gastroenteritis
- Tropical sprue
- Celiac disease
- Acquired immunodeficiency related complex
- Macroglobulinemia
Treatment and Management
Medical Treatment
The treatment primarily involves antibiotic medication and management of the symptoms, with the commonly prescribed medicines including:
- Ceftriaxone (Rocephin)
- Meropenem (Merrem I.V.)
- Penicillin G (Pfizerpen)
- Streptomycin (Streptomycin)
Your medicines and doses may need to be changed if you relapse during the treatment period of one to two years. Antimalarial medications and corticosteroids may also be suggested by your doctor. Surgery is not required in most cases.
Healthy Diet Choices
- Following a diet high in proteins as well as healthy calories (they help the body to better absorb nutrients)
- Having plenty of foods rich in iron (meat, eggs, leafy green vegetables), calcium (cheese, nuts, yogurt), magnesium (spinach, soybeans, and avocados) and vitamins ( especially A, B12, D, E and K)
To make up for nutrient deficiencies, your doctor may further recommend vitamin and mineral supplements.
Prognosis
Within the first or second week of taking the antibiotics, you are likely to get relief from the symptoms, while continuing them for a month usually ensures speedy recovery. However, there are around 40% chances of relapse, especially in high risk cases. Leaving the condition untreated may even lead to death.
ICD-9 and ICD-10 Codes
The ICD- 9- CM code of this disease is 040.2 and the ICD- 10- CM code is K90.81
References:
- http://www.mayoclinic.org
- https://www.niddk.nih.gov
- http://www.ncbi.nlm.nih.go
- http://www.healthline.com
- http://patient.info


Great info as I’m a person suffering from whipple’s disease at this present time it’s the worst thing I’ve ever experienced. I was a respiratory therapist for 10yrs in a Philadelphia based hospital and taught clinical through umdnj which is now rowan medical school. The only thing that is not accurate is that it is highly infectious and easily spread to other people I know because I’ve spread this to my ex wife, my two young boys, and other immediate family members. Just look up tropheryma whipplei and intrafamilial circulation and also read tropheryma whipplei causes epidemic fever in Senegal and you’ll see that I’m correct. This is an infectious bacteria so for anyone to think it’s not contagious must be crazy viruses are not contagious but bacteria are absolutely 100% contagious.
There will be an outbreak of this in our country if it hasn’t happened already. Europe is diagnosing patients with this on a regular basis. Also read about the 7 people they did a study on who thought they had arthritis which really turned out to be whipple’s disease in every case. The US needs to open their eyes and start testing and looking for this infection as a culprit causing many complications as it can spread to any and every system in our bodies. I do think alot of the cancers, autoimmune diseases, and even autism are being caused by this very bacteria. That and not very many people are aware of or familiar with it maybe that’s why doctors are so in the dark about it. I got this infection from a health supplement called deer antler velvet spray which came from New Zealand. I have dysautonomia and many other issues because of this underlying infection it has caused me permanent heart, nervous system, and brain damage. It’s deteriorated almost my entire body and every system in it. I also have hypothalamif dysfunction from it as well. This bacteria is some very nasty and intelligent stuff to go undetected for so long.