What is Scleritis?
Scleritis literally means the inflammation of the sclera, which is the outer white area of the eye. The sclera is responsible for providing the white color of the eye and maintaining the shape of the eye. This requires prompt diagnosis and treatment because it is a serious eye condition that may lead to possible vision loss.
This condition is usually associated with autoimmune disorders such as: Wegener’s granulomatosis, systemic lupus erythematosus and rheumatoid arthritis. Women are often affected with scleritis in association with some menstruation problems. There are other cases in which the cause of the condition is unknown. This is not a common disease, though it may be an early sign of some connective tissue diseases. [3]
Types of Scleritis
- Diffuse Scleritis. This involves the anterior portion of the sclera and is usually the most common type.
- Nodular Scleritis. This type involves the formation of nodules in the sclera.
- Necrotizing Scleritis. This type is usually the most severe of its kind and is most likely to result in the loss of vision. It is also known as scleromalacia perforans.
- Posterior Scleritis. This is considered the rarest type and involves the posterior area of the eye. Retinal detachment, closed angle glaucoma and muscular eye problems are the most common complications associated with this type.
Causes Of Scleritis
- Scleritis is often associated with an underlying disease that usually affects the body as a systemic condition. Generalized vascular disorders, connective tissue diseases and autoimmune disorders have been linked to half of the cases, especially those cases that have both eyes affected with the condition.
- Some cases have been linked to the presence of microorganisms like fungi, parasites, pseudomonas and viruses.
- Exposure to chemicals and trauma.
- About 30% of the cases of scleritis have unknown cause.
Signs and Symptoms of Scleritis
- The sclera may become red and swollen. In some cases, the sclera would turn into a purple hue.
- A severe, penetrating and ocular pain may be felt in the head and facial regions. The pain may radiate to the temple areas and jaw. Pain would usually result from the over stretching and stimulation of the nerve endings during inflammation.
- Photophobia or intolerance to light may also be felt. Pain is experienced when exposed to light.
- Tearing without purulent discharge usually occurs.
- Decreased visual acuity which may possibly lead to vision loss.
Scleritis Pictures

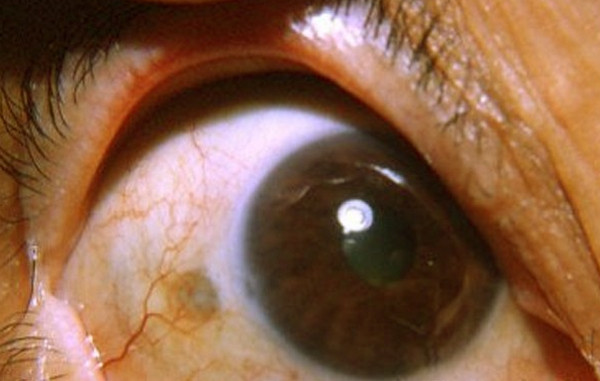
Picture 1 : Scleritis image
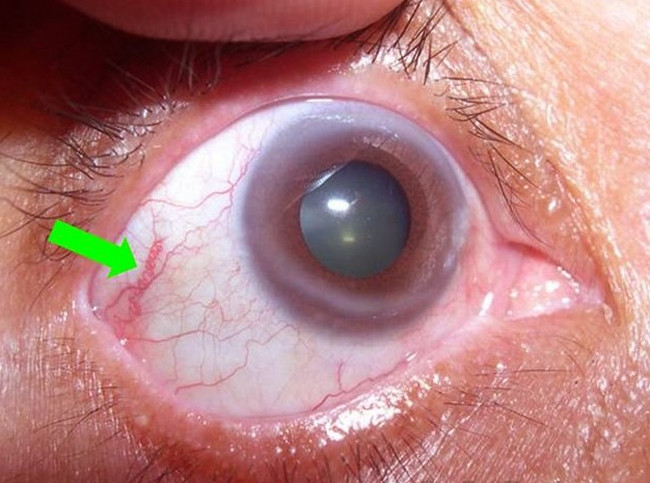
Picture 2 : Scleritis
Picture 3 : Scleritis photo
Diagnosis and Work Up
- Physical examination of the eye under broad daylight is important in determining scleritis. This can be done by retracting the eyelids to determine the involvement of the surrounding areas of the sclera.
- Visual acuity testing is done through the Snellen eye chart or the metric acuity test.
- Slit lamp examination is done to examine the internal structures of the eyes like the eyelids, sclera, conjunctiva and the iris. No special preparation is required prior to the procedure. [5]
- Eye drops, however, may be used to dilate the pupils 15 to 20 minutes prior to the actual examination of the eyes. In addition, the eye drops should also be used with caution because it may cause an increase in the intraocular pressure.
- Phenylephrine or neosynephrine eye drops may be used to differentiate episcleritis from scleritis. The blood vessels may appear blanched in episcleritis and not in scleritis. Episcleritis is the inflammation of the outer layer of the sclera.
- Computed tomography (CT) scan, ultrasonographies and magnetic resonance imaging (MRI) may also be used in examining the eye structure.
Treatment for Scleritis
- Scleritis is best managed by treating the underlying cause. Different causes of the underlying condition require specific therapy.
- Eye surgery is necessary in cases of necrotizing scleritis. Damaged corneal tissue would need to be repaired to preserve eye function and prevent further eye deterioration, which may lead to vision loss. Scleral grafts may be used and can be obtained through eye banks.
- Oral medication like corticosteroids may be indicated to suppress inflammation especially if the case is associated with an autoimmune disorder.[6]
- In less severe cases, non-steroidal anti-inflammatory drugs like ibuprofen may be used to relieve pain.
- Oral antibiotics may be prescribed if it is thought to be infectious.
- Chemotherapy may be used for more aggressive cases. Methotrexate (MTX) is usually the first drug of choice for chemotherapy. Cyclophosphamide or azathioprine may also be used.
- Subconjunctival steroid injections may also be used if systemic side effects of certain drugs are causes of concerns.
Complications Associated with Scleritis
- Severe vision loss or blindness is probably the worst complication. This can happen if scleritis is left untreated.
- Keratitis and uveitis are also possible. Keratitis is the inflammation of the cornea of the eye while uveitis refers to the inflammation of the uveal tract of the eye. The uveal tract includes the iris, choroid and ciliary body.
- Cataract, glaucoma, retinal swelling may also develop as complications.
- Cataract and glaucoma may occur as a result of long term use of corticosteroid eye drops.
Prognosis for Scleritis
Scleritis is a serious eye condition that needs prompt and aggressive diagnosis and treatment to prevent worsening and deterioration of the condition, which may eventually lead to blindness. It has the tendency to be recurrent. Therefore strict compliance with the medications is necessary. In addition, the underlying condition needs to be diagnosed and treated properly to eliminate the chances of recurrence and to prevent further complications.
In most cases, preventive treatment is not available. However, patients with underlying conditions which have scleritis as one of its complications should be informed regarding the risks and possible development of the condition.
Successive consultation with the ophthalmologist and other specialists involved in treating the systemic condition should also be done regularly. This is to monitor and evaluate the recurrence of scleritis as well as the autoimmune disorder. In addition, the patient should be properly educated regarding the facts associated with scleritis and the underlying condition.
References:
- http://emedicine.medscape.com/article/1228324-followup#a2645
- http://www.nlm.nih.gov/medlineplus/ency/article/001003.htm
- http://en.wikipedia.org/wiki/Scleritis
- http://www.medicinenet.com/scleritis/article.htm
- http://www.medicinenet.com/scleritis/page3.htm#how_is_scleritis_diagnosed
- http://www.rightdiagnosis.com/s/scleritis/treatments.htm
- http://vision.about.com/od/sportsvision/p/Scleritis.htm
- http://emedicine.medscape.com/article/809166-overview

I worked with test equipment associated with the US Navy years ago. I have developed arthritis of the eye, Scleritis and arthritis of the head. With early electronics there were several harmful insulators use in the wiring etc. I am sure we worked with asbestos.
I was wondering if you have heard of any links between these?