Pyelonephritis
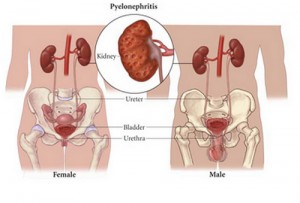
The kidneys are bean-shaped structures in the abdominal cavity that are roughly the size of a human fist. They are one of the most important excretory organs of the body. These renal structures are located at the paravertebral gutter, lying at a retriperitoneal position.
The basic unit of this excretory organ is the nephrons – responsible for filtering blood and removing the body’s waste products. These renal structures are complex reprocessing structures that filter approximately 190 liters of blood and process 2 liters of metabolic wastes and excess water per day. The surplus water and wastes would become urine that is stored in the bladder until released through urination. Aside from excreting wastes, the kidneys also secrete three essential hormones: rennin (helps control blood pressure), erythropoietin (promotes production of red blood cells at the bone marrow), and calcitriol (active type of Vitamin D for bone calcium maintenance).
The right kidney is normally at lower position than the left due to the asymmetry of the liver. The right kidney lies behind the liver while the left kidney is behind the spleen. Both kidneys are positioned underneath the diaphragm. Each kidney weighs 127 to 170 grams in males and 115 to 155 grams in females.
These structures are divided into two sections: the outer renal cortex and the inner renal medulla. The blood needed by the organs is supplied by the renal arteries. Once blood has been filtered, it goes back to the heart through the renal veins.
The surfaces of the kidneys are enclosed by a transparent capsule (renal capsule) that would protect it from trauma and infection. These surfaces vary as one part is convex and the other is concaved where the renal pelvis is attached. The pelvis extends to the ureters.
What is Pyelonephritis
A serious ascending bacterial urinary tract infection of the kidneys is termed pyelonephritis. Escherichia coli is the most common causative agent of this infection. Other bacteria that can trigger the kidney infection are Pseudomonas, Proteus, Streptococcus faecalis and Staphylococcus aureus. The renal pelvis and the interstitial area are the primary areas affected. There are different types of pyelonephritis:
Acute Pyelonephritis
The sudden occurrence of pelvis and renal parenchyma inflammation that is characterized by yellowish marks and small abscesses at the cortex that is due to the buildup of pus in the interstitial tissue and collecting tubules.
Chronic Pyelonephritis
This condition is brought about by recurring renal infection. This condition occurs practically in patients with anatomic anomalies as well as with struvite calculi, urinary tract obstruction, vesicoureteral reflux (most common) or renal dysplasia. This is linked to scarring of the renal tissues and would eventually progress to end-stage renal disease. Intrarenal reflux of contaminated urine has been suggested to cause renal injury that would lead to scar formation when healed.
Xanthogranulomatous Pyelonephritis
This is an uncommon inflammatory state due to the constant obstruction in the kidneys because of nephrolithiasis (usually staghorn calculus) and would result to irreparable damage of the renal parenchyma. Diabetic individuals are more predisposed to this disease. Histologic analysis of the inflamed mass would reveal macrophages that are full of lipids and inflammatory cells. The condition is more common in females, infants and white children less than two years old.
Emphysematous Pyelonephritis
This is a severe, life-threatening, necrotizing kidney infection that affects the renal parenchyma. It is characterized by the presence of gas formations in the perirenal tissues, parenchyma and collecting system, postulated to be consequent to glucose fermentation. The disease is frequent in people with uncontrolled diabetes and occurs six times more in women and in individuals between ages 19 and 81. The clinical signs of this disease are comparable to acute pyelonephritis but can be fatal if not treated immediately. A high incidence of mortality (about 50%) is associated with this kind of pyelonephritis.
Pyelonephritis in Pregnancy
This mainly happens during the fifth to seventh months. Pregnant women are prone to develop this problem since the reduced bladder and ureteral tone plus the increasing bladder volume would contribute to increased uterovesical reflux and urinary stasis. A lot of pregnant women would have glycosuria which might promote growth of bacteria in the urine. The increasing urinary estrogens and progestins would lessen the resistance of the lower urinary tract to invading bacteria causing urinary tract infection. If left untreated, it can cause maternal sepsis, early labor causing the premature delivery of the baby.
Pyelonephritis in Children
Polynephritis is children are usually due to perianal contaminants (bowel flora) but those affecting neonates are understood to be hematogenous in nature. The colonization of bacteria would likely be due to urinary stasis of low-flow incidents. This may be due to irregular voiding, obstruction, incomplete voiding or vesicoureteral reflux (about 33% in children). This condition would occur at any stage but in the neonates, pyelonephritis is more common in boys – which are largely associated with renal tract abnormalities. Uncircumcised males have higher prevalence. But as children grow, this condition will be more prevalent in females.
Pyelonephritis Symptoms
Acute pyelonephritis symptoms are systemic and the first indications would include high fever, flank pain, joint and muscle pains, headache and if severe, delirium might be present. Symptoms might develop rapidly in acute cases.
Other symptoms of pyelonephritis would include:
- Dysuria
- Polyuria
Nocturia - Hematuria or pyuria
- Foul-smelling urine
- Renal colic (if due to presence of stones)
- Uncontrollable shivering
- Nausea and vomiting
- Diarrhea
- Hypotension (if sepsis has occurred)
- Poor feeding, jaundice, irritability in infants
- Urinary urgency
- Anorexia
Some individuals do not show any symptoms of pyelonephritis at all. In the elderly, confusion or changes in the mental status would be the early sign of the presence of the disease.
Pyelonephritis Causes
Pyelonephritis is can be caused by the following:
- Bladder infection
- Prolonged use of catheter
- Use of cystoscope for urethral and bladder examination
- Urinary tract surgery
- Nephrolithiasis that causes blockage
- Urinary stasis
- Anatomical abnormalities of the urinary system
- Urinary Tract Infection that is left untreated
- Diabetes
- Bladder tumor
- Neurogenic bladder problems
- Urine reflux
- Enlarged prostate
- Pregnancy
- Spermicide use
- Multiple partners
- Immunocompromised states
Pyelonephritis Diagnosis
Positive leokocytes and nitrites seen in the urine dipstick exam that manifest the characteristic symptoms is enough to diagnose pyelonephritis. Formal diagnosis is by urine culture and if the origin of the infection is uncertain, then blood cultures are needed.
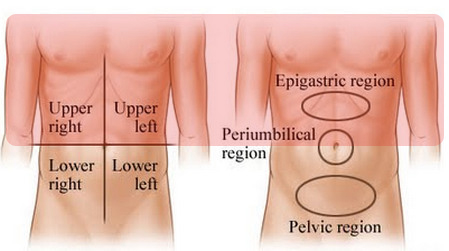
In order to rule out any underlying disorders, abdominal CT scans and intravenous pyelograms are done. The following conditions would need additional diagnostic exams:
- Intense flank pain characteristic of renal colic
- No response to at least two days antibiotic therapy
- Recurring symptoms just after the antibiotic regimen
- Chronic pyelonephritis
- Men
Abdominal ultrasound or the helical computed tomography studies could possibly reveal structural abnormalities, urinary obstruction or presence of kidney stones. Sometime there are cases that would need kidney biopsy and voiding cystourethrogram.
Acute pyelonephritis would also need contrast nephrograms while the xanthogranulomatous type would need additional exams such as urography.
Pyelonephritis Pathology
Pyelonephritis is a suppurative, exudative localized inflammation of the kidney. The renal parenchyma exhibits abscesses that consist of pus, fibrin, neutrophils, hematoxylinophils and cell debris. Gross pathology would show pathognomonic suppuration and impression of hemorrhage at the renal pelvis and cortex. For chronic pyelonephritis, scarring and fibrosis are present.
The pathogenesis of the disease condition begins with attachment of the uropathogenic E. coli to the renal epithelium that would activate the body’s inflammatory response. This would release the chemokines (Interleukins) and chemotactic and allow polymorphonuclear leukocytes to cross the barrier (epithelial) into the urine. Bacterial phagocytosis in the urine occurs at pH 6.5 to 7.5 and with an osmolality of 485 mosM. If the urine has less than these values, the phagocytosis is significantly reduced.
When pyelonephritis gets complicated, the host defenses are down, thus the probability of infection is increased. Additional urinary stasis would provide a good medium for bacterial growth. Spermicide prevents lactobacilli growth which generates hydrogen peroxide. Frequent intercourse would cause mechanical trauma to the urethra while diabetes can develop autonomic bladder neuropathy, leukocyte dysfunction, glucosuria, nephrosclerosis and microangiopathy.
Pregnancy would increase the risk for developing upper UTI. Progesterone would reduce ureteral peristalsis and increase the capacity of the bladder but the growing uterus would shift the bladder position and contributes to stasis of urine.
Pyelonephritis Treatment
Since the main cause of the problem is infection, then antibiotic treatment is the mainstay of this condition. Minor cases may use oral antibiotic therapy though at the initial phase of the treatment, intravenous fluids are used (give loading doses). The kind of antibiotics that will be used would depend on the local practice and may comprise of fluoroquinones, beta-lactam, trimethoprim or nitrofurantoin. Aminoglycosides are combined for a brief period because of their toxicity. Severe cases may necessitate the use of the intravenous antibiotics to counteract the insensible loss from elevated temperature, vasodilation and decreased oral intake; and to improve urine output.
Structural abnormalities or obstruction may need surgical intervention. Individuals with Xanthogranulomatous Polynephritis would need nephrectomy (removal of kidneys) because of the high possibility of recurrent infections.
References:
http://kidney.niddk.nih.gov/kudiseases/pubs/pyelonephritis/
http://emedicine.medscape.com/article/245559-overview
http://www.merckmanuals.com/home/sec11/ch149/ch149d.html